1.‘I wasn’t exercising before I fell pregnant, so I can’t exercise now’
Wrong! *throws her hands up in the air in exasperation*
The energy used during a ‘average’ labour is similar to the energy burnt during a half marathon. You wouldn’t go into a half marathon without any training would you? Now, I’m not saying that you should start running 10km a day if you weren’t before you fell pregnant, but, if you have been cleared by your doctor to exercise then start exercising (morning sickness permitting)! 2.5 hours of moderate intensity exercise per week can provide these benefits for the mother:
- Reduced back and pelvic pain
- Improved constipation
- Decreased risk of caesarian delivery, pre-eclampsia and gestational diabetes
- Decreased excess weight gain
- Weight loss after the baby is born
- Improved overall fitness, mood and general discomforts
- And these benefits for the baby:
- Decreased fat mass
- Improved behavioural maturation
- Improved stress tolerance
2.‘I must keep my heart rate at 140bpm when exercising whilst pregnant’
This is quite an ‘old school’ way of thinking. The American College of Obstetricians and Gynecologists regularly update their guidelines for exercising during pregnancy, and they ditched the heart-rate monitor years ago. Your heart capacity changes through each trimester, so a stock-standard heart rate target is not applicable. Instead, use the Borg Scale (rating of perceived exertion):
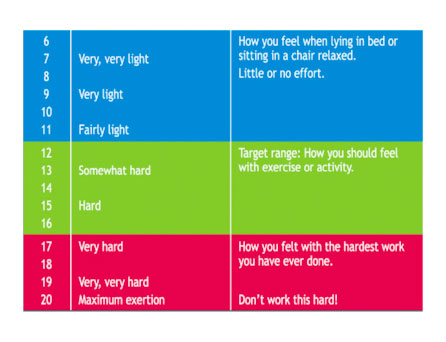
Moderate intensity on the Borg Scale is somewhere between 12-14, feeling like you’re exercising ‘somewhat hard’, kind of like brisk walking. Or, use the talk test: where you have a bit of huff and puff going on, but could still have a short conversation with someone.
3.‘I can’t work my abdominals now that I’m pregnant’
This is kind of half wrong. You have 4 layers of abdominals. Your top layer (the six pack muscle) separates during pregnancy to allow for growth of the baby (more on this in a later blog post). To prevent too much separation, avoid working this muscle excessively. Exercises or movements to avoid:
- Crunches/sit ups
- Full planks
- Double leg lifts/lowers when lying on your back
- Any exercise where you feel strain through your upper tummy muscles
However, your deepest layer of muscle (transversus abdominus) acts like a corset around your spine, abdomen and tummy and provides stability for your lower back, pelvic joints and helps your pelvic floor do its jobs. This muscle is being stretched more and more every day of pregnancy, so needs to be strengthened to prevent back and pelvic pain! See your physio for basic Pilates based exercises to perform.
 4.‘Exercising causes early miscarriage, early labour, and smaller babies’
4.‘Exercising causes early miscarriage, early labour, and smaller babies’
There are several studies proving that this statement is not true. Exercise is good for mother and baby during pregnancy! However, some forms of exercise needs to be modified. Furthermore, if you have cervical insufficiency (short cervix), twins/triplets with risk of pre-term labour, aneamia (low iron), high blood pressure, placenta previa (a low lying placenta), lung or heart issues, you must consult with your doctor prior to exercising.
Some fantastic forms of exercise when pregnant:
- pilates
- pregnancy yoga
- stationary bike riding
- swimming/aqua-aerobics
- brisk walking (if you don’t have pelvic girdle pain)
- light weights
Please read the American College of Obstetricians and Gynecologists website for more information on exercise during pregnancy: http://www.acog.org/Patients/FAQs/Exercise-During-Pregnancy
5. ‘I’ll just get back into my normal exercise regime straight after I deliver’
It all depends of what your normal form of exercise is. If it is low impact exercise, then start it at around 4-6 weeks post natal (depending on mode of delivery). However, if you usually perform high impact exercise, it’s best to explore the low impact options in the ‘fourth trimester’ after giving birth. Pregnancy and childbirth is a huge event on a woman’s body. Compare childbirth with a knee reconstruction on an All Black rugby player – the athlete will have a period of rest and recovery for 6 weeks, then perform knee specific rehab with his physio, and probably won’t be back on the field until 9-12 months later. Childbirth is pretty similar! Your body (particularly the pelvic floor) needs to have relative rest and recovery for the first 6 weeks. Your pregnancy hormones are still affecting your connective tissue until 12 weeks post natal, and your breastfeeding hormones have an effect on connective tissue too. During this time, you are more prone to musculoskeletal injury, and also to vaginal prolapse and incomplete pelvic floor healing. So, high impact exercise (running, heavy weights, contact sports) is best avoided for 12 weeks, and should only be resumed once cleared by your pelvic floor physio.
Being a bit of a feminist myself, I do struggle to advise against running or high impact sports in the early post natal days, because us women can do anything right?! But really, it’s only a short time of a woman’s life, and an opportunity to explore new or alternate forms of pelvic floor safe exercise, in order to decrease the risk of incontinence, prolapse, joint pain and more. Here are some pelvic floor friendly forms of exercise:
- Post-natal yoga
- Post-natal pilates
- Swimming
- Spin classes/bike riding
- Light weights
- Brisk walking
– the vagina physio

